
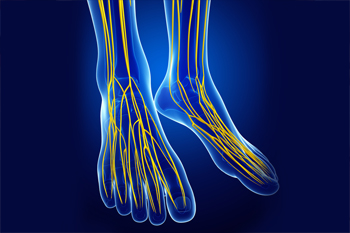
 Tarsal tunnel syndrome is a nerve disorder in which the posterior tibial nerve, located near the heel of the foot, is compressed. This is usually caused by participating in repetitive activities, such as running or jumping, that put stress on the nerve and surrounding areas. However, it can also be the result of a trauma, having flat feet, or being overweight. Tarsal tunnel syndrome causes foot and ankle pain, burning, tingling, and numbness. The pain usually worsens while walking and can improve with rest. There are several treatments for tarsal tunnel syndrome, including resting and icing the affected leg, taking oral pain medications, injecting steroids into the area, immobilizing the leg, wearing an orthotic, or physical therapy. In more severe cases, surgery may be needed to decompress the posterior tibial nerve. If you are experiencing the symptoms of tarsal tunnel syndrome, please seek the care of a podiatrist.
Tarsal tunnel syndrome is a nerve disorder in which the posterior tibial nerve, located near the heel of the foot, is compressed. This is usually caused by participating in repetitive activities, such as running or jumping, that put stress on the nerve and surrounding areas. However, it can also be the result of a trauma, having flat feet, or being overweight. Tarsal tunnel syndrome causes foot and ankle pain, burning, tingling, and numbness. The pain usually worsens while walking and can improve with rest. There are several treatments for tarsal tunnel syndrome, including resting and icing the affected leg, taking oral pain medications, injecting steroids into the area, immobilizing the leg, wearing an orthotic, or physical therapy. In more severe cases, surgery may be needed to decompress the posterior tibial nerve. If you are experiencing the symptoms of tarsal tunnel syndrome, please seek the care of a podiatrist.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact one of our podiatrists of Achilles Foot Clinic. Our doctors can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
The Effects of Tarsal Tunnel Syndrome
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions, please feel free to contact one our office, located in the South of Calgary, Alberta. We offer the newest diagnostic and treatment technologies for all your foot care needs.
Tarsal tunnel syndrome is a condition in which there is a compression of the posterior tibial nerve. The posterior tibial nerve runs along the inside of the ankle into the foot. Tarsal tunnel syndrome is named for the tarsal tunnel, which is a thin space along the inside of the ankle beside the ankle bones. This space contains various nerves, arteries, and tendons, and includes the posterior tibial nerve. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome the tibial nerve is compressed, causing tingling or burning, numbness, and pains.
Common causes of tarsal tunnel syndrome involve pressure or an injury. Injuries that produce inflammation and swelling in or around the tunnel may place pressure on the posterior tibial nerve. Direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or trauma to the tibial nerve, can result in tarsal tunnel syndrome. Diseases that damage nerves, such as diabetes or arthritis, may cause tarsal tunnel syndrome. Those with flat feet are at risk for developing the condition, as the extra pressure and strain placed on the foot may compress the posterior tibial nerve.
Feeling different sensations in the foot at different times is a common symptom of tarsal tunnel syndrome. An afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg. Symptoms are primarily felt on bottom of the foot and/or the inside of the ankle. Symptoms can appear suddenly and may occur due to overuse of the foot.
To diagnose tarsal tunnel syndrome, your podiatrist may examine the foot and tap the posterior tibial nerve to see if symptoms surface. He or she may also order an MRI to determine if a mass is present.
Treating tarsal tunnel syndrome will depend on the decision of your podiatrist. Multiple options are available, however, and can include rest, ice, immobilization, oral medications such as anti-inflammatory drugs (NSAIDS), physical therapy, injection therapy, orthotics, supportive shoes, braces, and surgery.
While there are several different types of flatfoot, all of them involve a loss of the arch—either partial or total. Flexible flatfoot is a common form of this condition where the arch collapses upon standing and returns to normal when there is no weight on the foot. Because having flat feet changes the alignment of the foot (toes point outwardly, the heel points toward the outside of the foot, and the ankle turns in), people with this condition may be more prone to developing bunions and hammertoes. Flexible flatfoot may cause pain in various areas of the foot including the arch, heel, ankle, shin bone, or on the lateral side of the foot. Additionally, there may be some pain in the knee, hip, or lower back, and overall fatigue or aching in the feet or legs. A podiatrist can diagnose flatfoot through an examination and by taking an X-ray. Non-surgical treatment may involve shoe modifications, physical therapy, losing weight, modifying activities, or even wearing ankle or foot orthoses to help support your arches and adjust your gait. For a proper diagnosis and to determine what treatment option is best for you, it is suggested that you visit a podiatrist.
Flatfoot is a condition many people suffer from. If you have flat feet, contact one of our podiatrists from Achilles Foot Clinic. Our doctors will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions, please feel free to contact one our office, located in the South of Calgary, Alberta. We offer the newest diagnostic and treatment technologies for all your foot care needs.
Flatfoot is a foot condition in which the arch of the foot has either partially or totally dropped or has never developed. While it is common in babies and small children, it can become a problem for them in adulthood if the arch never forms. For adults, the development of flat feet can be brought upon by injury, as a result of pregnancy due to increased elasticity, or obesity. Those who have health concerns such as rheumatoid arthritis or diabetes may also be at greater risk for developing the condition.
If you suspect that you have flat feet, it is best to consult your podiatrist. Your foot doctor will examine the suspected foot and observe how it looks while you sit and stand. He or she may take an X-ray to determine how serious the condition is. Some common signs of flatfoot include toe drift, in which the toes and front part of the foot point outward, a short Achilles tendon, and a heel that tilts outwardly while the ankle tilts inward.
Once flatfoot has been diagnosed, your podiatrist may suggest one of several treatment options. Flat feet can be rigid, in which the feet appear to have no arch even when the person is not standing; or flexible, in which the person appears to have an arch while not standing, but once standing the arch disappears. Those with flexible flatfoot may be told to reduce any activities that cause pain and to avoid extended periods of walking or standing. Another suggestion may be weight loss, as excessive weight may be placing pressure on the arches
In few cases, if the condition is severe and all other methods have been exhausted surgery may be required. This is normally avoided, however, due to a lengthy recovery time and high cost.
 You may not pay a lot of attention to your feet on a normal basis. However, showing your feet some love with basic foot care and the right footwear will help you avoid a variety of foot and ankle problems. Keep your feet clean, and always dry them fully before putting on socks to avoid fungal infections. Nails should be trimmed regularly and properly: straight across and not so short that they dig into the sides of the toe and possibly cause an ingrown toenail. Only wear shoes that are fitted properly and offer good heel and arch support, with enough room at the toe box for your toes to move around. High heels are not suggested and should not be worn every day, and block heels or kitten heels are better than stilettos. Ill-fitting shoes and the prolonged stress of high heels on your feet and toes can cause a variety of foot and ankle conditions. Inspect your feet as you are drying off from showering every day. If you notice any lesions, changes in appearance, or have any discomfort or pain, contact a podiatrist.
You may not pay a lot of attention to your feet on a normal basis. However, showing your feet some love with basic foot care and the right footwear will help you avoid a variety of foot and ankle problems. Keep your feet clean, and always dry them fully before putting on socks to avoid fungal infections. Nails should be trimmed regularly and properly: straight across and not so short that they dig into the sides of the toe and possibly cause an ingrown toenail. Only wear shoes that are fitted properly and offer good heel and arch support, with enough room at the toe box for your toes to move around. High heels are not suggested and should not be worn every day, and block heels or kitten heels are better than stilettos. Ill-fitting shoes and the prolonged stress of high heels on your feet and toes can cause a variety of foot and ankle conditions. Inspect your feet as you are drying off from showering every day. If you notice any lesions, changes in appearance, or have any discomfort or pain, contact a podiatrist.
Everyday foot care is very important to prevent infection and other foot ailments. If you need your feet checked, contact one of our podiatrists from Achilles Foot Clinic. Our doctors can provide the care you need to keep you pain-free and on your feet.
Everyday Foot Care
Often, people take care of their bodies, face and hair more so than they do for their feet. But the feet are a very important aspect of our bodies, and one that we should pay more attention to. Without our feet, we would not be able to perform most daily tasks.
It is best to check your feet regularly to make sure there are no new bruises or cuts that you may not have noticed before. For dry feet, moisturizer can easily be a remedy and can be applied as often as necessary to the affected areas. Wearing shoes that fit well can also help you maintain good foot health, as well as making it easier to walk and do daily activities without the stress or pain of ill-fitting shoes, high heels, or even flip flops. Wearing clean socks with closed shoes is important to ensure that sweat and bacteria do not accumulate within the shoe. Clean socks help to prevent Athlete’s foot, fungi problems, bad odors, and can absorb sweat.
If you have any questions, please feel free to contact one our office, located in the South of Calgary, Alberta. We offer the newest diagnostic and treatment technologies for all your foot care needs.
Our feet are arguably one of the most important parts of the body. When it comes to health and beauty routines, the feet and toenails are usually ignored. You should always practice proper footcare to avoid any fungal infections or ailments that can not only ruin the appearance of your feet, but also cause pain. Ignoring any foot problems could potentially lead to an expensive doctor’s visit.
The most important step in proper foot care is to wash your feet daily. You should wash them with soap and water. Doing this will cleanse your feet of dirt, sweat and bacteria. It is crucial that you clean between the toes and pat your feet dry with a towel afterward. Your toenails are also an important part of the feet and you may find that they get dirtier in the summer when you wear sandals. It is important that you practice proper toenail care in addition to cleaning the rest of your feet. When trimming your nails, you should always trim straight across instead of in a rounded shape. Trimming in a curved shape may lead to ingrown toenails.
Moisturization is also important for foot care, and you should be moisturizing your feet every day. The best way to prevent dry feet is to rub lotion or petroleum jelly on your clean feet at night and put socks over them. In the morning, your feet should be soft and moisturized.
Another crucial step in proper foot care is to wear the right shoes for whichever activity you are going to partake in. In warmer weather, you should wear shoes that allow your feet to breathe. It is best to avoid shoes such as flip-fops that do not provide arch support. Tight shoes may also be harmful, and they may even cause you to develop bunions.
If you plan on taking a shower in a public area, you should be especially careful, so you do not pick up any fungi. Showers are prone to harboring different types of bacteria and fungi. You should always wear shower shoes or flip flops when walking around in locker rooms and public showers. Avoid sharing shoes with other people because this is another way that fungus may be spread.
If you are experiencing any problems with your feet you should speak with your podiatrist to determine the best method of treatment for you.
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
 Foot wounds, or ulcers, occur when the outer layers of the skin are damaged, thus exposing the deeper tissues of the feet. Ulcers can form due to wearing shoes that don’t fit correctly or from an injury that breaks the skin. Ulcers are most common in patients who have diabetes, neuropathy or vascular disease, and these open wounds can become infected if left untreated. While the wounds may not be painful, common signs include redness, inflammation, an odor, or thickened tissue. Patients who are at a higher risk for foot wounds, or have wounds that don’t heal, should consult with a podiatrist. Usually, a podiatrist will remove the unhealthy skin to assist with healing. Then, depending on the situation, special shoe padding, antibiotics, or surgery may be recommended for treating the wound.
Foot wounds, or ulcers, occur when the outer layers of the skin are damaged, thus exposing the deeper tissues of the feet. Ulcers can form due to wearing shoes that don’t fit correctly or from an injury that breaks the skin. Ulcers are most common in patients who have diabetes, neuropathy or vascular disease, and these open wounds can become infected if left untreated. While the wounds may not be painful, common signs include redness, inflammation, an odor, or thickened tissue. Patients who are at a higher risk for foot wounds, or have wounds that don’t heal, should consult with a podiatrist. Usually, a podiatrist will remove the unhealthy skin to assist with healing. Then, depending on the situation, special shoe padding, antibiotics, or surgery may be recommended for treating the wound.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with one of our podiatrists from Achilles Foot Clinic. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact one our office, located in the South of Calgary, Alberta. We offer the newest diagnostic and treatment technologies for all your foot care needs.